Featured News
Academy Statement
July 11, 2025
National Academies Presidents Express Alarm Over Unnecessary Suffering and Deaths Caused by Measles Outbreak
Academy Statement
June 16, 2025
National Academies Launch Restructuring
Academy Statement
June 11, 2025
Importance of Science in Decision-Making About Vaccines
Press Release
June 2, 2025
S7 Statements: Advancing Science for Society
In the News
May 27, 2025
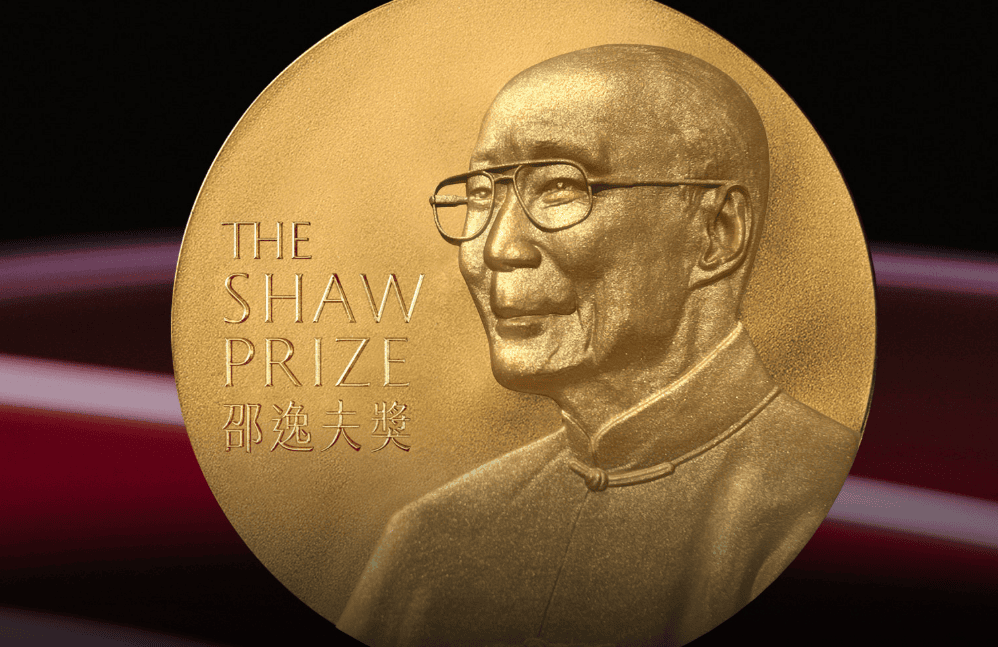
NAS International Members Honored with Shaw Prize
May 19, 2025
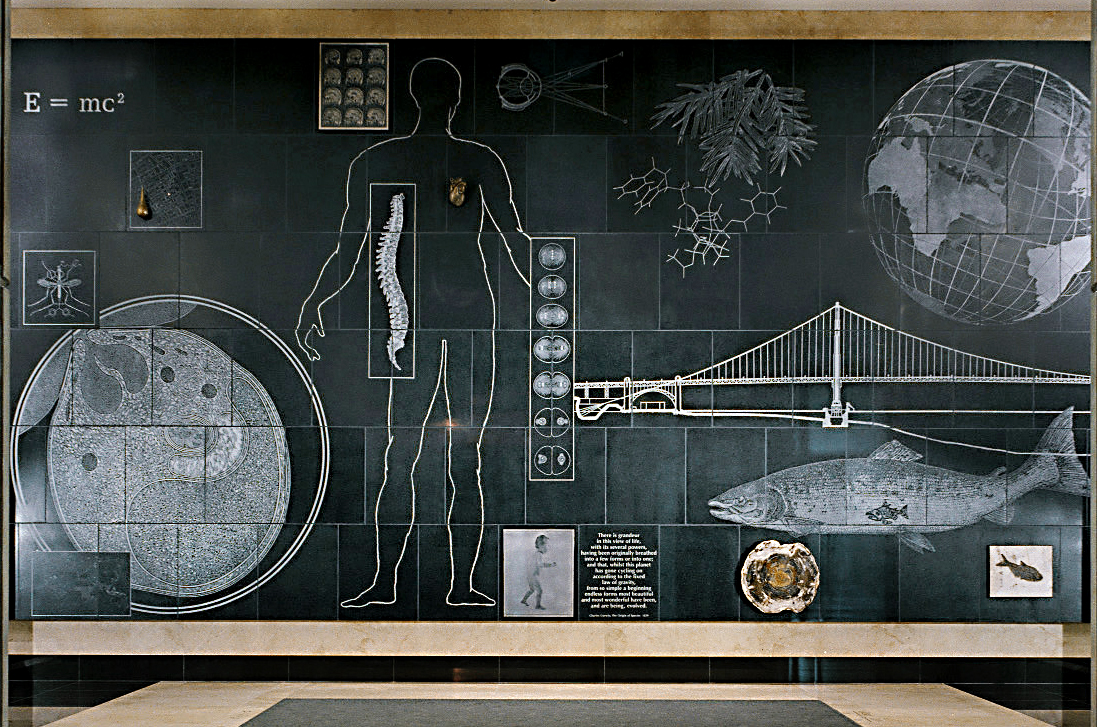
OSTP Director Speaks at NAS
Press Release
May 5, 2025
NAS President Marcia McNutt to Deliver Second State of the Science Address on June 3
News from the National Academies
News and features from the National Academies of Sciences, Engineering, and Medicine (NASEM).