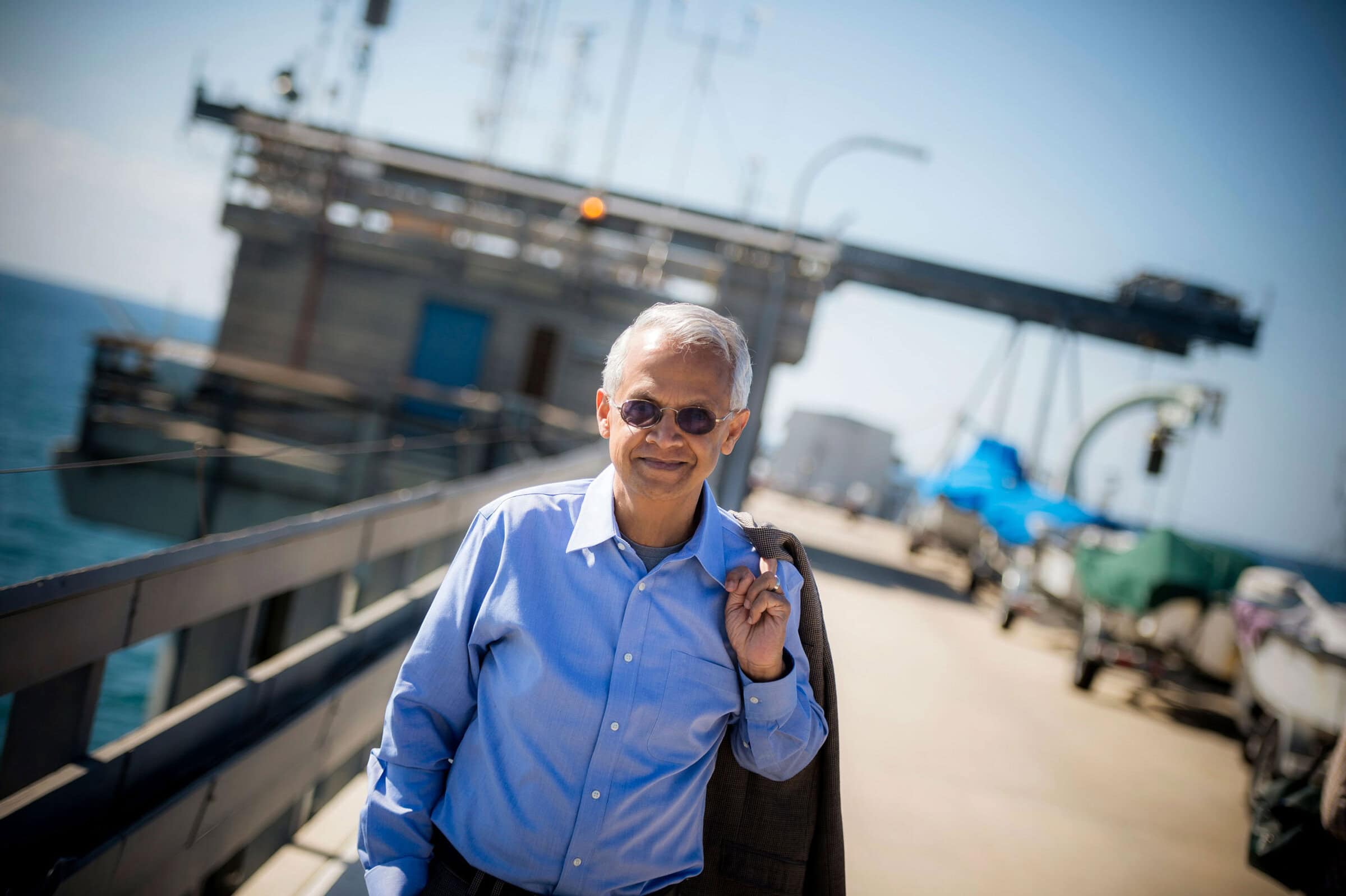
On World Diabetes Day, pioneering physician-scientist E. Dale Abel reflects on a career spent uncovering how diabetes affects the heart and blood vessels. From uncovering the molecular mechanisms that drive diabetic heart disease to advancing strategies for prevention and treatment, Abel’s research continues to shape the future of diabetes care and inspire progress toward a healthier world. In this Q&A, he shares how new research is paving the way toward prevention, earlier interventions, and more equitable access to care worldwide.
Your work has transformed our understanding of diabetic heart disease. What first drew you to study the intersection of diabetes and cardiovascular health?
My doctoral thesis as Rhodes Scholar in Oxford was focused on understanding the emerging concept at the time of cardiometabolic disease in humans, with an emphasis on the relationship between insulin resistance and hypertension. This interest was further sparked as an Endocrinology Fellow at the Beth Israel Deaconess Medical Center at Harvard, where I sought training in molecular tools that would enable the modeling of metabolic physiology in gene-modified mouse models. Some of my early studies were examining the impact of altered glucose transport and insulin signaling in the heart. These initial studies sparked my interest to further pursue fundamental mechanisms that could explain the pathophysiology of increased heart failure risk in diabetes. As these studies evolved over my career, we extended our work to examine mechanisms beyond the heart, to include the role of altered insulin signaling, metabolism, and mitochondrial dysfunction, in contributing to vascular and platelet dysfunction in diabetes.
How has the field of diabetes research changed most significantly over the course of your career?
It is challenging to capture the exponential increase in knowledge that has taken place in diabetes research in the past three decades. We have much more insight into molecular mechanisms that lead to beta cell dysfunction, mechanisms linking obesity to insulin resistance and diabetes, increased insights into the pathophysiology of diabetes complications, advances in diabetes technology, which has transformed the care of patients with type 1 diabetes and of course the discovery, characterization, and ultimate deployment of GLP1R agonists, which have transformed the landscape of diabetes and obesity therapeutics. There have also been advances made in more accurate phenotyping of diabetes with the goal of developing more personalized approaches to diabetes treatment and prevention.
What scientific development in the last 5–10 years gives you the most hope for reducing the global impact of diabetes?
The work of epidemiologists linking obesity and sedentary lifestyles to the acceleration in type 2 diabetes prevalence is really important. Insights revealing the possibility of reversing or significantly delaying the onset of type 2 diabetes by addressing underlying precipitating risk factors such as obesity underscores the notion that there could be an important subset of diabetes that could be prevented, with a greater focus on healthy nutrition at global scale. Approaches that will increase our ability to identify specific risks (molecular, genetic, societal) that will predict transition to diabetes, could lead to the deployment of early and effective treatment and preventive strategies. The development of new therapies that impact many diabetes complications such as cardiovascular and renal disease should provide the opportunity to enable subjects with diabetes to live healthier and longer lives. Many of these agents remain too expensive for global deployment, thus focusing on equity and access to agents represents an important global imperative.

What emerging areas of research do you believe will reshape diabetes prevention or treatment in the next decade?
What is the contribution of inter-organ crosstalk in the pathophysiology of diabetes and its complications? There is growing evidence implicating inter-organ communication in metabolic regulation, which if understood could lead to more targeted strategies for prevention and treatment of those at risk for diabetes and its complications. Specifically, by identifying and targeting these pathophysiologically relevant biomarkers, we might move towards more precision-based diagnostics, risk modeling and ultimately treatment not only of diabetes, but its complications.
What are the biggest barriers that still prevent cutting-edge diabetes research from reaching patients, especially in underserved communities?
An important and often not recognized barrier to the deployment of research advances, particularly to underserved communities, is a lack of appreciation for how social determinants of health also drive diabetes pathophysiology. As new diabetes technologies and therapies are confirmed to be effective, there needs to be parallel economic analyses of the benefits of early and effective treatment versus the costs of complications, to rebalance the way in which all payors of healthcare, governmental and otherwise, can be encouraged to recognize the value proposition that investments in health made now, may reduce escalating expenses later.